A quarter-century ago, the populist premier of the day wanted to fix nursing homes in Ontario.
Mike Harris had a lasting impact on long-term care when his Progressive Conservatives oversaw the expansion of private ownership in a sector short on regulations and standards. Harris, having spearheaded for-profit ownership back then, now profits handsomely from it himself.
Today, as
chair of Chartwell Retirement Residences, the former premier presides over a sprawling operation that describes itself as “the largest retirement living company in Canada.” Didn’t know that?
Neither, says Doug Ford, did he.
Replying to my questions Monday, our current premier said he’s spoken to the former premier but once, briefly, during this pandemic. Long-term care, where the majority of
COVID-19 deaths have taken place in this province, never came up.
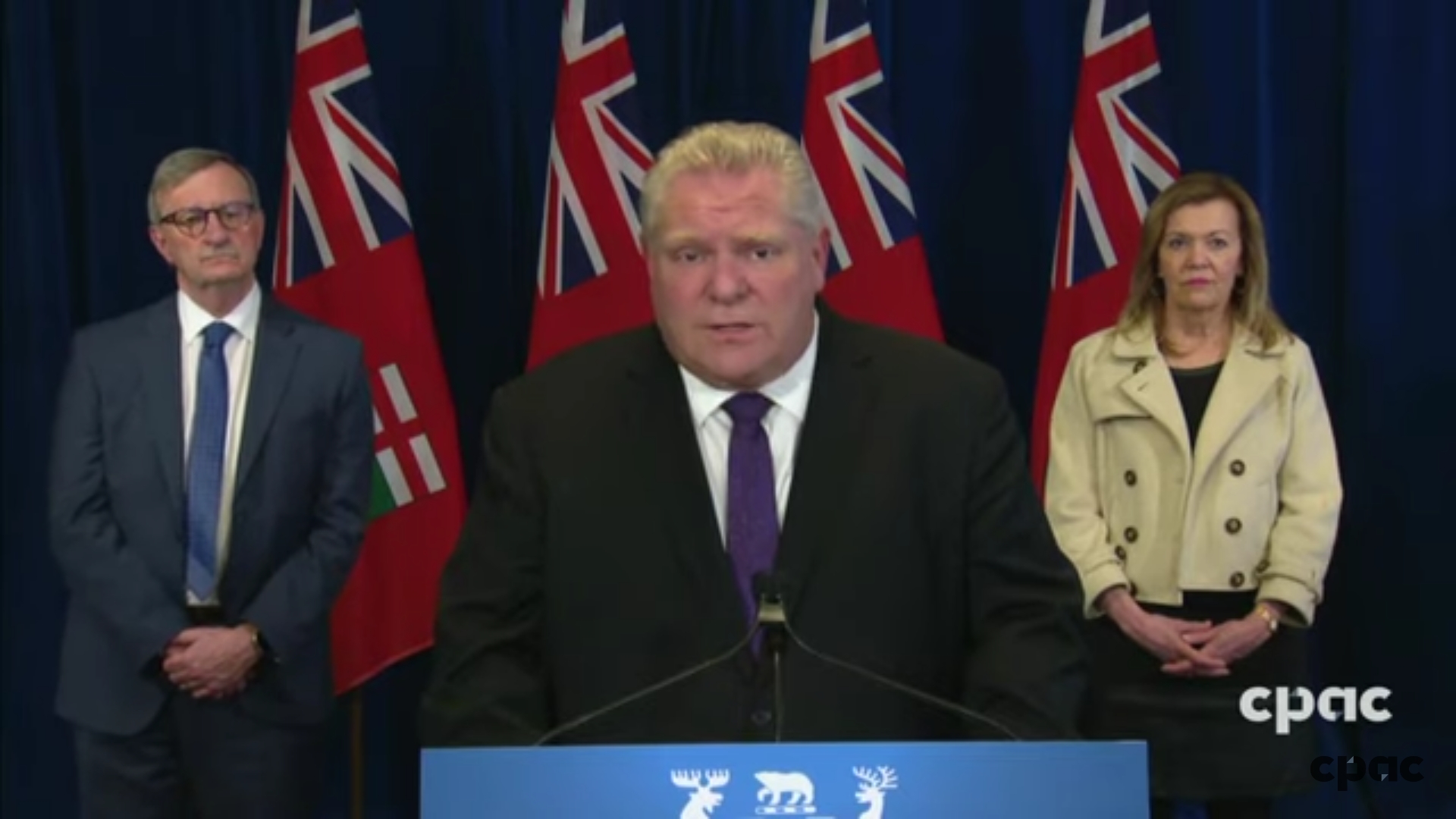
“He asked how I was doing and to be frank, I didn’t even know he was the chair of Chartwell,” Ford told me in his televised daily briefing, where he often rattles off the names of CEOs whom he encourages do their best in the pandemic.
I’d asked Ford if he had an opinion, as premier, about the difference between public and private ownership, given the carnage in long-term care today. The premier took a quick pass at the topic before passing on it.
“Well, I think there’s a difference, but what I’ve said right from the day one, Martin, the system’s broke and we are going to fix it. But if you don’t mind, Martin, I’m going to pass it over to the minister of long-term care.”
But did Ford have a message for Harris or other operators involved in
long-term care in Ontario?
“We’re gonna have that opportunity to sit down and fix these issues right across the board,” he replied. As for Harris, “the conversation lasted a couple of minutes — ‘How’s your family doing?’ ‘How’s yours?’ — and that was about it.”
One wonders, when family came up, if Ford mentioned the thousands of other families that have been affected in this crisis (he has mentioned publicly that his own mother-in-law became infected with COVID-19 in a Toronto nursing home last month).
Today, from his perch as chair, Harris is well placed to look back at what he kick-started from the premier’s chair, and see how it ended up. But Ford is in a better position to take a fresh look at what his predecessor did — and, with the benefit of hindsight, to re-examine the system he inherited.
Privatization predated Harris, just as
many problems predated Ford. But the Tories back then made it easier for owners by easing staff ratios and requirements, just as the Tories last year scaled back annual comprehensive inspections.
The premier says he’ll “fix it.” Harris had a fix, too.
Ford says “there’s a difference” between for-profit ownership versus non-profit. Harris presumably thought so, too, but what’s the difference between their views?
After Ford mentioned they’d chatted, I reached out to Harris for comment, to which a Chartwell spokesperson replied: “Mr. Harris has confirmed that Mr. Ford’s statement is correct and there is nothing additional to add.”
There are few quick fixes, because our long-term care crisis has been a long time coming: Private versus non-profit or public ownership? Single rooms versus double or triple? Nursing home homes versus home care?
One solution is to stop low-wage, part-time workers flitting from one facility to another, as a way to reduce infection transmission between homes. Yet it took weeks for the Progressive Conservative government to impose the ban (a loophole allowed for temporary help as needed).
And at precisely that time, Ford invited health-care workers from acute-care hospitals and army clinics to swoop in on nursing homes. Physicians frequently go from private clinics to nursing homes, acting as involuntary vectors of infection.
Separation surely saves lives, but a living wage with decent working conditions might spare us the need for SWAT teams from hospitals and medics from army bases. Either way, we won’t know for a while how profound the differences were in infection control between profit-seeking owners and non-profits.






/https://www.thestar.com/content/dam/thestar/politics/provincial/2020/03/06/ford-government-to-abandon-hard-to-read-blue-licence-plates-and-return-to-a-white-design/licence_plate.jpg)